The 2022 monkeypox (MPX) outbreak first came to public attention in a way that eerily echoed the earliest days of COVID-19, as an obscure story that did not receive much front-page treatment. Media reports shared that a British resident who had travelled to Lagos and Delta State in Nigeria, in areas where MPX is considered to be an endemic disease, came down with a painful rash on April 29 while still in Africa. He flew back to the U.K. on May 4, and felt so ill that he was admitted to a hospital later that day. At Guy’s Hospital in London, he tested positive for MPX on May 6.
A paper just published in the peer-reviewed journal The Lancet Infectious Diseases suggests that MPX had already spread far beyond Nigeria by the time that U.K. individual had returned to his homeland. In the paper, lead author Daniele Lapa and colleagues document what happened to a 39-year-old man from Italy who travelled in Austria during the first two weeks of May 2022. “He self-identified as an MSM (which the CDC holds refers to gay, bisexual, and other men who have sex with men) and sex worker and reported condomless sexual intercourse with several male partners during the previous month.” He was HIV-positive, and “reported a history of sexually transmitted infections.” He too was admitted to a hospital, in Italy, nd diagnosed with MPX. While there, he said that he had received one dose of smallpox vaccination during childhood, more than 30 years earlier.
Even just considering these two cases, it is not hard to see how an infectious disease—however initially established—can spread beyond country borders and to many different individuals. The organization Think Global Health has compiled a detailed timeline of emerging developments from the beginning of the 2022 MPX outbreak. It gives a sense of how the infectious viral disease ballooned to over 26,000 cases worldwide as of early August: https://tinyurl.com/4cbjzw63
Why Is MPX Spreading Now?
Cases of MPX outside of Africa since May 7 of this year have exceeded the overall number of cases detected outside of endemic areas from 1970 to the current outbreak. “The newest rate of human infections is even more alarming when we consider that cases in the last two months vastly exceeded the number of confirmed or suspected human monkeypox cases in the entire 20th century,” according to Aileen Marty of Florida International University’s Division of Internal Medicine.
The stories of the two aforementioned men, in terms of their traveling and general lifestyles, are nothing new. Many others before them have gone on similar travels and engaged in comparable behaviors. What then has changed to expand community transmission of MPX in 2022? Marty reviewed studies on MPX and wrote this month in The Lancet Microbe that mutational changes in the circulating MPX virus might provide an advantage in human hosts such that there is “improved viral replication,” “improved evasion of innate defense mechanisms,” “improved evasion of adaptive defense mechanisms,” “improved stability outside of a host,” and more.
Still other researchers believe that the end of routine vaccination against smallpox, which in the U.S. happened in 1972 after the disease was then-eradicated in the states, contributed to the present situation here.
A Vaccine for Smallpox and a Drug Stockpiled Due to Bioterrorism Fears
For several years, the CDC has categorized smallpox—a viral zoonosis with a virus closely related to that which causes MPX—as a Category A Bioterrorism Agent/Disease. This means that it:
MPX fatality rates conversely at present are low, ranging from 0–11% in outbreaks in endemic areas, with mortality mostly affecting younger children and severe disease primarily impacting immunocompromised individuals, according to the European Center for Disease Control and Prevention. Nevertheless, concerns over smallpox helped drive the development of Jynneos, which is the CDC’s preferred vaccine to protect against MPX. It is manufactured by Bavarian Nordic, a biotech company with headquarters in Denmark.
On August 9, the CDC reported: “Globally and in the United States, supply of Jynneos vaccine is currently limited, although more is expected in the coming weeks and months. In the United States, there is a large supply of ACAM2000, but this vaccine has more side effects and contraindications.”
If you read about the side effects and problems associated with ACAM2000, it is evident why the focus is on Jynneos now (https://tinyurl.com/mr395mpd ).
In terms of medication to treat MPX, the world’s first approved smallpox drug was fast-tracked by the Trump Administration back in 2018. Interest in the antiviral medication called TPOXX was fueled by concerns over “U.S. health security” and to “prepare for the potential use of smallpox virus in bioterrorism attacks against the U.S.,” according to a U.S. Department of Health and Human Services (HHS) news release at the time. The HHS then stockpiled TPOXX and supported development of an IV formulation of the drug.
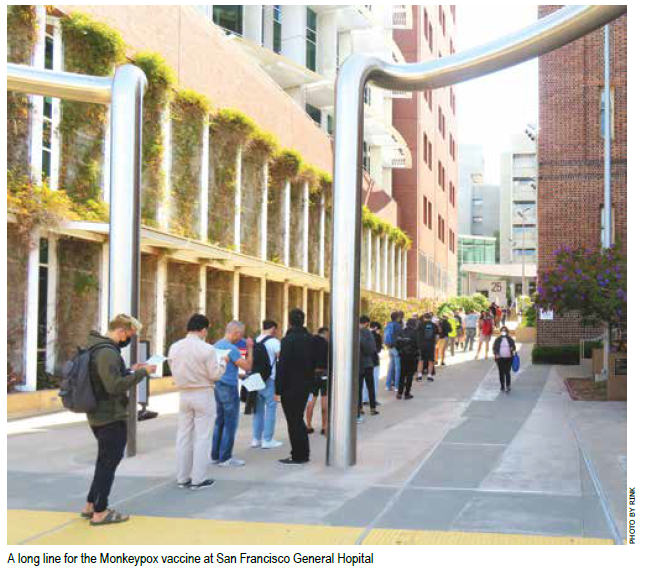
All of this history now comes to the forefront, as many people the world over are now attempting to receive the Jynneos vaccine and, if infected with the MPX virus, to receive doses of TPOXX.
State Senate Oversight Hearing on Monkeypox
On August 9, 2022, State Senator Scott Wiener (D-San Francisco), Chair of the Senate Select Committee on Monkeypox, convened an oversight hearing on MPX. Shortly before the hearing, he shared: “Monkeypox is a public health emergency, and we must do everything in our power to expand access to vaccination, testing, treatment, and information. We need to listen to those who have contracted monkeypox, healthcare providers, public health officials, and advocates on the ground. Working together, we can protect our community’s health.”
The hearing included remarks from leaders such as state epidemiologist Erica Pan, Dr. Vivek Jain—an HIV and infectious diseases specialist from San Francisco General Hospital, Dr. Grant Colfax—Director of Health, City & County of San Francisco, Dr. Muntu Davis—County Health Officer for the Los Angeles County Department of Public Health, Dr. Tyler TerMeer of the San Francisco AIDS Foundation, and several others.
The hearing brought to light problems and concerns that go beyond the MPX illness itself, such as when Amber Parrish Baur, Executive Director of the UFCW Western States Council, spoke about how individuals can be financially impacted by MPX. Many San Franciscans, for example, have experienced long lines attempting to obtain the vaccine, often causing hours of lost work time and pay. There is already unprecedented strain on healthcare workers, including pharmacists, she added.
Dr. TerMeer expressed the frustration shared by many over delays—particularly at the federal level—concerning testing, vaccination, treatment, and more. He said that there was a “lack of urgency” concerning MPX in the days preceding Pride Month as well as “an inadequate vaccine supply,” leading him and others to feel “abandoned by inaction.”
Some individuals who have contracted MPX shared their stories during the hearing. San Francisco resident David Watson, for example, told how he contracted the virus via casual contact: he hugged and quickly kissed a friend upon meeting up with him. The friend had no idea that he was infected. He had a small bump on his face that he thought was just an ingrown hair.
Frustration as Officials Weigh Guidance at Local, State, and Federal Levels
Discussed at the hearing was the FDA’s just-announced emergency use authorization that permits healthcare providers to change how the Jynneos vaccine is administered—giving it intradermally (between layers of skin) rather than subcutaneously. Providers can then get five doses out of a standard one-dose vial, stretching out the now-limited supply of the vaccine.
The San Francisco Department of Public Health shared this statement in response with the San Francisco Bay Times:
“We are committed and open to explore every possible avenue that would allow us to get more people vaccinated against monkeypox as soon as possible. SFDPH is awaiting federal and state guidance on the changeover from subcutaneous to intradermal injections of Jynneos vaccine, including FDA instructions on dose extraction and administration, and CDPH instructions on how to account for and register each dose when multiple doses are taken from single vials. We are also aware that the intradermal method of administering the vaccine, in which a dose is injected between layers of skin, will require updated protocols and additional training for many vaccinator staff and may be slower to administer. SFDPH needs to understand adjustments that would need to be made to operations to ensure San Francisco’s vaccine providers continue to reach as many people who need the vaccine as quickly and equitably as possible. We will provide further updates to the community as appropriate.”
It therefore remains in question when the FDA’s new approach might be implemented in San Francisco. The good news, at least for now, is that the Zuckerberg San Francisco General Hospital monkeypox vaccine clinic has reopened, thanks to a vaccine replenishment of 10,000 doses, and is scheduled to be open at least through this Saturday, August 13.
Fast Action Needed to Curb MPX Spread
A protest co-organized by San Francisco Bay Times columnist Joanie Juster and attended by LGBTQ community leaders and members of the public on August 8, 2022 in San Francisco called for “cutting the red tape” and moving faster both to treat those with MPX and to curb the illness’ spread. Many health officials are calling for similar action. As an international team led by Dr. Hamna Raheel of the Dow University of Health Sciences recently wrote in the Annals of Medicine and Surgery: “The COVID-19 pandemic should be a pressing reminder for the health sector to act promptly against monkeypox transmission. The virus’ spread via respiratory droplets should not be underappreciated when compared to the aerosol droplet spread of COVID-19. Appropriate measures to quickly isolate and quarantine patients presenting with symptoms is a compelling need. A spillover infection like monkeypox is highly virulent with subsequent mutations surfacing, monitoring its epidemiology henceforth is imperative.”
For More Information About MPX
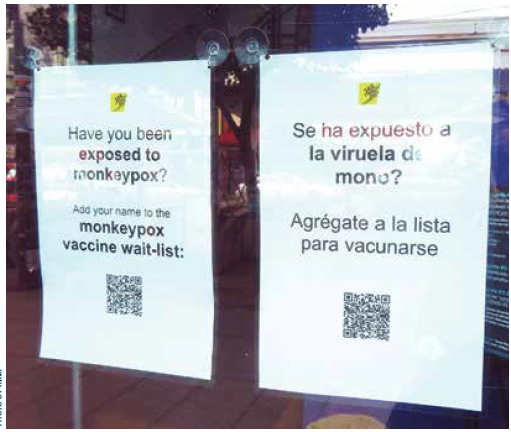
San Francisco Department of Public Health: for status of vaccine availability, answers to common questions (under FAQ), and monkeypox case numbers and demographics – https://tinyurl.com/ym2zt54j
San Francisco AIDS Foundation: for SFAF’s testing, diagnosis, and treatment services – https://tinyurl.com/3jzjp4rz
Published on August 11, 2022
Recent Comments